The U.S. Food and Drug Administration (FDA) has approved two gene therapies, Casgevy and Lyfgenia, for the treatment of sickle cell disease (SCD) in patients aged 12 years and older. This marks a significant milestone in the field of gene therapy, as Casgevy is the first FDA-approved treatment to utilize CRISPR/Cas9 genome editing technology.
SCD is a group of inherited blood disorders that affect approximately 100,000 people in the U.S. The therapies aim to address the primary problem in SCD, which is the sickling of red blood cells. Casgevy modifies patients' hematopoietic stem cells using CRISPR/Cas9 to increase the production of fetal hemoglobin, thereby preventing the sickling of red blood cells. On the other hand, Lyfgenia genetically modifies patients' blood stem cells to produce HbAT87Q, a gene-therapy derived hemoglobin that functions similarly to normal adult hemoglobin.
While the approval of these therapies is a cause for celebration, concerns have been raised about their accessibility and affordability. Further research is also needed to monitor potential long-term effects. The therapies have shown promising results in clinical trials, freeing patients from severe pain crises. However, there are concerns about the long-term risks, logistical challenges, and access to these intensive procedures.
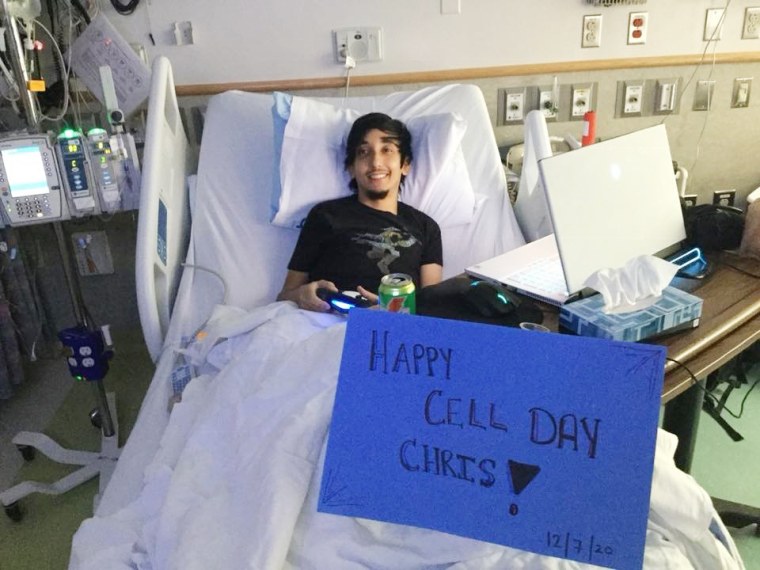
One case highlighted is that of Johnny Lubin, a 15-year-old who has lived with sickle cell disease since infancy. Lubin underwent a cutting-edge clinical trial involving gene editing, which involved removing stem cells from his bone marrow, using CRISPR technology to increase the amount of protective hemoglobin, and then infusing the edited cells back into his bloodstream. This case represents the potential of these therapies to improve the lives of patients with SCD.