In a significant development, new studies suggest that the Human Papillomavirus (HPV) vaccine not only prevents cervical cancer in women but also reduces the risk of head and neck cancers in men. The HPV vaccine has been shown to protect against strains of the virus linked to various types of cancer, including those affecting the throat and mouth.
According to a study published in BMJ, England's HPV vaccination program has led to a significant decrease in cervical cancer and grade 3 cervical intraepithelial neoplasia (CIN3) across socioeconomic groups. The highest reduction was observed among females with the highest vaccination uptake and youngest age at immunization.
Another study, published in the American Society of Clinical Oncology conference, found that HPV vaccination rates among males have been increasing and lag behind those of females but are accelerating. The researchers noted that men are about twice as likely to develop head and neck cancers than women, making this a crucial development.
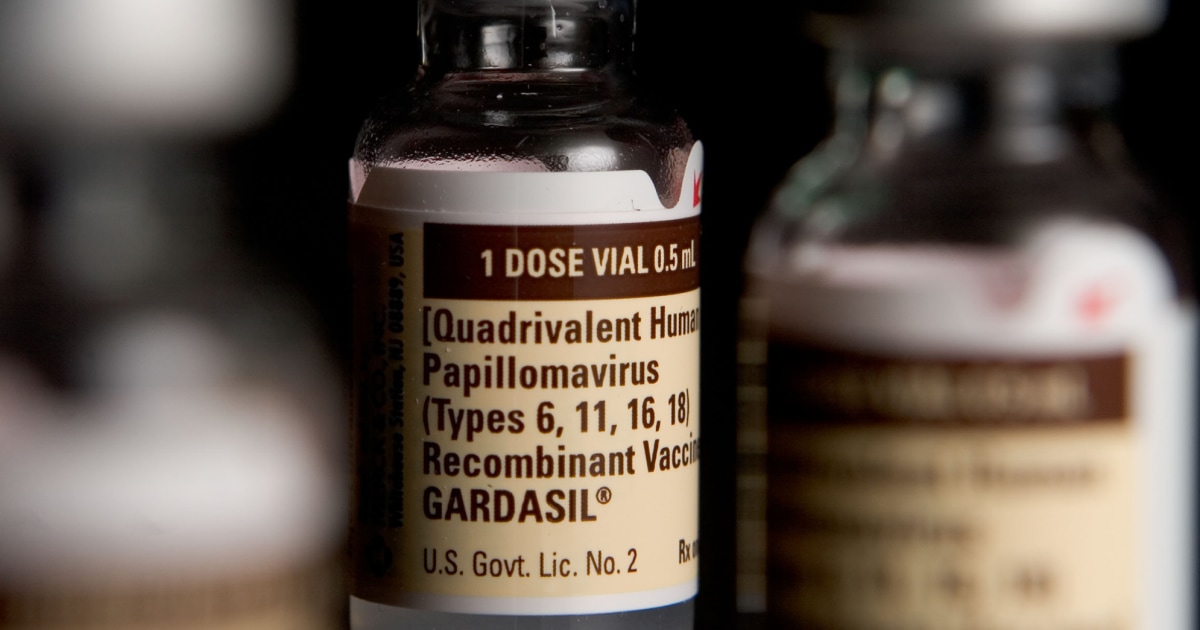
The Centers for Disease Control and Prevention (CDC) recommends HPV vaccination for adolescent boys since 2011, with catch-up shots available for anyone through age 26 who hasn't been vaccinated. The vaccine has been shown to protect against strains of the virus linked to cervical cancer and has significantly reduced rates of this cancer.
The HPV vaccine is also effective in preventing penile, anal, and vaginal cancers. A study published in Stat News reported that no cases of cervical cancer were found in women who were vaccinated before they were 14 years old. The researchers noted that the highest decrease in cervical cancer and CIN3 was observed among females with the highest vaccination uptake and youngest age at immunization.
Despite these findings, HPV vaccination rates among adolescents and young adults in the US have improved from 7.8% to 36.4% for males and from 37.7% to 49.4% for females between 2011 and March 2020.
Merck's sales of the HPV vaccine grew by 29% to $8.9 billion in the last year, indicating a growing awareness and acceptance of the importance of HPV vaccination.
It is important to note that while these studies suggest a significant reduction in cancer risk associated with HPV vaccination, more research is needed to fully understand its long-term effects and potential benefits.
Sources:
- BMJ: Effect of the HPV vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia by socioeconomic deprivation in England: population based observational study.
- Stat News: New data show the HPV vaccine prevents cancer in men, too. Why don't more people get it?
- Time: HPV Vaccines Prevent Cancer in Men as Well as Women


