Parkinson's Disease: New Blood Test Predicts Seven Years Before Symptoms Appear
Recent research has shown promising results in the development of a blood test that can predict Parkinson's disease (PD) up to seven years before symptoms appear. The test, which uses artificial intelligence to identify a panel of eight blood biomarkers, may revolutionize the way we diagnose and treat this debilitating neurodegenerative disorder.
According to studies published in various scientific journals, researchers have identified 23 distinct proteins that are consistently dysregulated in patients with PD compared to healthy controls. Six of these proteins were also shown to be dysregulated in patients with premotor isolated REM sleep behavior disorder (iREM), a condition that is often a precursor to PD.
The model was able to identify 100% of the patients with PD based on the expression of these eight biomarkers and predict which patients with iREM would convert to PD with an accuracy of 79%. Most of these markers robustly correlated with clinical scores on the Unified Parkinson's Disease Rating Scale and Mini-Mental State Examination.
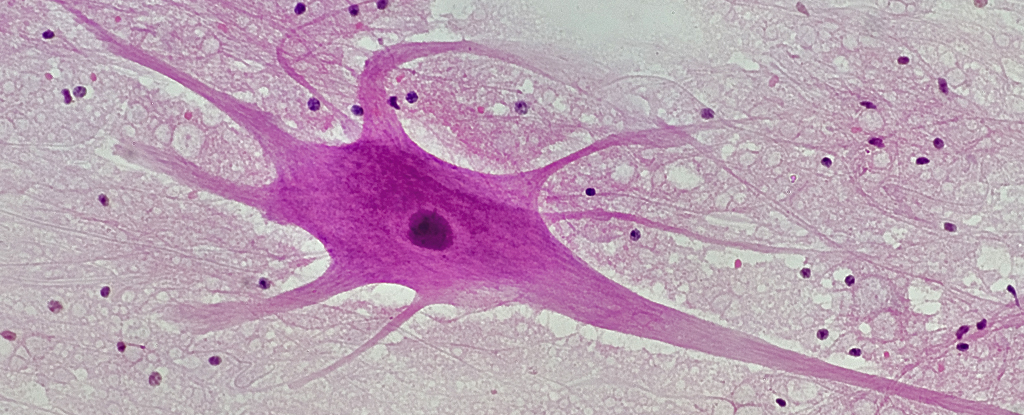
The potential implications of this discovery are significant. Currently, there is no cure for PD, and no treatment can slow or stop its progression. Symptoms include tremors, low movement, stiffness and tension in muscles, difficulty moving around or making facial expressions. The main cause of PD is the loss of nerve cells in the brain that produce dopamine due to the build-up of a protein called alpha-synuclein.
Early diagnosis is crucial for effective treatment and management of PD. With this new blood test, researchers hope to identify patients at risk before they develop symptoms, enabling them to enroll in clinical trials of treatments aimed at slowing or halting the disease process.
The development of a simple and non-invasive diagnostic tool for PD is an exciting prospect for both patients and healthcare professionals. It could lead to earlier intervention, improved quality of life, and potentially even preventative measures. However, larger trials are needed to validate the accuracy of this test in a broader population.
Sources:
- Nature Communications: Plasma proteomics identify biomarkers predicting Parkinson's disease up to 7 years before symptom onset
- Science Alert: New Test Detects Parkinson's 7 Years Before Most Symptoms Show



